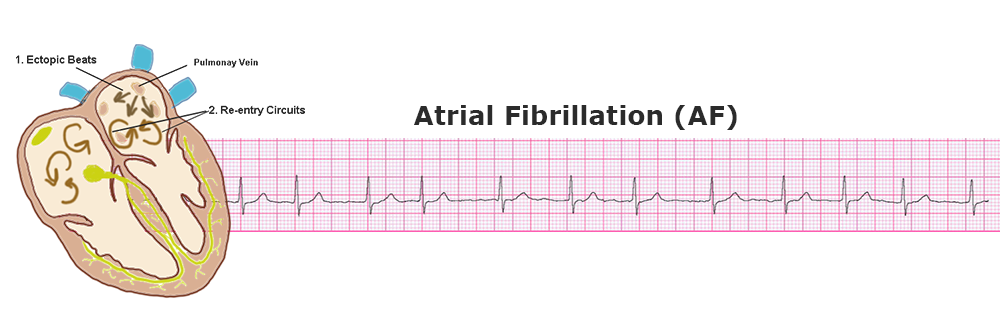
Atrial fibrillation is a very common arrhythmia worldwide. It is caused by both cardiac as well as non-cardiac etiologies. There is a ton of literature on AF, however in this post, I will give you top ten very useful points, which will be definitely helpful in exams as well as during your clinical practice.
Tip # 1 - Digoxin in AF
Digoxin is a positive inotropic agent, that is used in AF treatment. It provides short-term symptomatic relief. It improves left ventricular ejection fraction (LVEF), improves dyspnea and thus will decrease the frequency of hospitalizations. However, it has not been shown to improve mortality, thus it is not a first-line treatment.
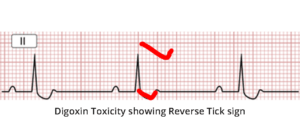
Since the therapeutic index of digoxin is narrow, serum digoxin levels should be checked periodically when it is used. In the presence of digoxin toxicity, ECG will show a characteristic ST segment depression, which typically looks like a mirror image of tick mark (reverse tick mark).
Features of digoxin toxicity include:
GI symptoms – Nausea, vomiting, abdominal pain, anorexia.
CNS symptoms – Visual disturbances, and disorientation.
Cardiac signs – Ventricular ectopics, AV block, and Atrial fibrillation itself.
Tip # 2 - Goals in the treatment of AFib
Treatment of AFib have mainly 3 main goals:
1- Decide whether to go for rate control or rhythm control.
2- Assess need for anticoagulation.
3- Search for an underlying cause of AF and its management.
Tip # 3 - Target Heart Rate (THR) in AF
At rest, Goal of rate control is to keep the heart rate below 90/minute.
During exertion, calculate THR by subtracting age (years) from 200. The result value will be the maximum acceptable heart rate during exertion.
Target heart rate (THR) during exertion in AF (bpm) = 200 – Age (in years)
Tip # 4 - Drugs used for Rate Control
Beta-blockers & rate-limiting (non-dihydropyridine) calcium-channel blockers (such as verapamil and diltiazem), are the drugs of first choice. If these fail, then add digoxin, and then amiodarone.
Tip # 5 - Digoxin as monotherapy. When?
Digoxin as monotherapy in chronic AF is acceptable only in sedentary patients, and is very beneficial in AF with systolic heart failure.
Tip # 6 - Combining Beta blockers & CCBs
Never combine beta-blockers and non-dihydropyridine calcium channel blockers. Such combination can potentially cause severe heart block.
Tip # 7 - Rhythm control: Drug of Choice
If rhythm control in AF is considered with a drug (termed as pharmacological cardioversion), the drug of choice is Flecainide.
The use of Flecainide is contraindicated, however, in patients with structural heart disease. In such patients, Amiodarone can be used.
Tip # 8 - AF > 48 hours
If the duration of AF is > 48 hours, elective cardioversion should be postponed until after 3 weeks of anticoagulation. This is to prevent the risk of cardio-embolization.
Tip # 9 - Consideration before anticoagulation
When considering anticoagulating the AF patient, calculate CHA2DS2-VASc score.
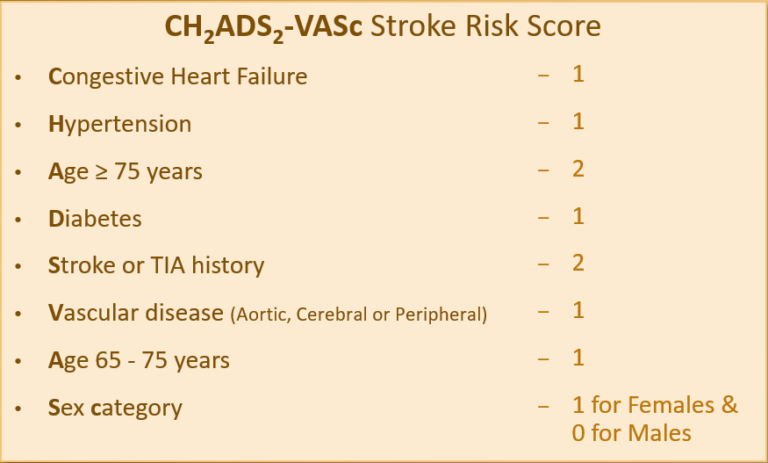
If CHA2DS2-VASc score is 2 or more, anti-coagulation is indicated.
Important note: The CHA2DS2-VASc score is not meant for AF in valvular heart disease patients. These patients are anticoagulated, anyway.
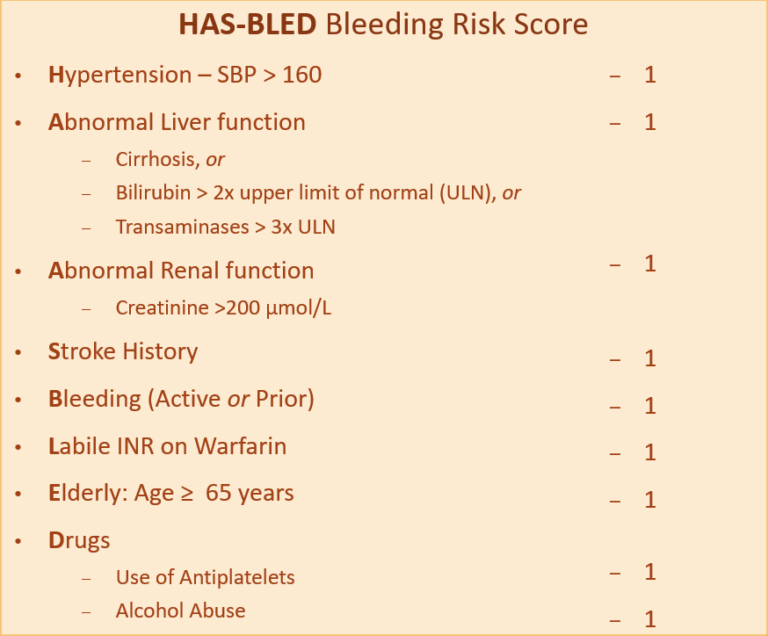
To evaluate for the risk of bleeding risk with anticoagulation, the HAS-BLED score is beneficial (figure below).
If the score is 3 or more, the patient has an increased risk of bleeding. A decision is based on the risk-benefit ratio of anticoagulation.
Tip # 10 - Anticoagulants in Valvular Heart Diseases
Do not use Direct oral anticoagulants (DOACs) in patients with valvular heart disease. Use warfarin, instead.
How did you find this post? Was it useful?
Please share your thoughts in the comments section.