According to the updated (2018) NICE guidelines on the management of chronic obstructive pulmonary disease (COPD), the management of stable COPD includes the following pertinent features:
General Management
- Provide smoking cessation advice, including offering nicotine replacement therapy, Varenicline, or Bupropion.
- Influenza vaccination – annually
- Pneumococcal vaccination – one dose
- Pulmonary rehabilitation for all people who are functionally disabled by COPD (Medical Research Council [MRC] for dyspnea grade 3 and above) and people who have had a recent hospitalization for an acute exacerbation.
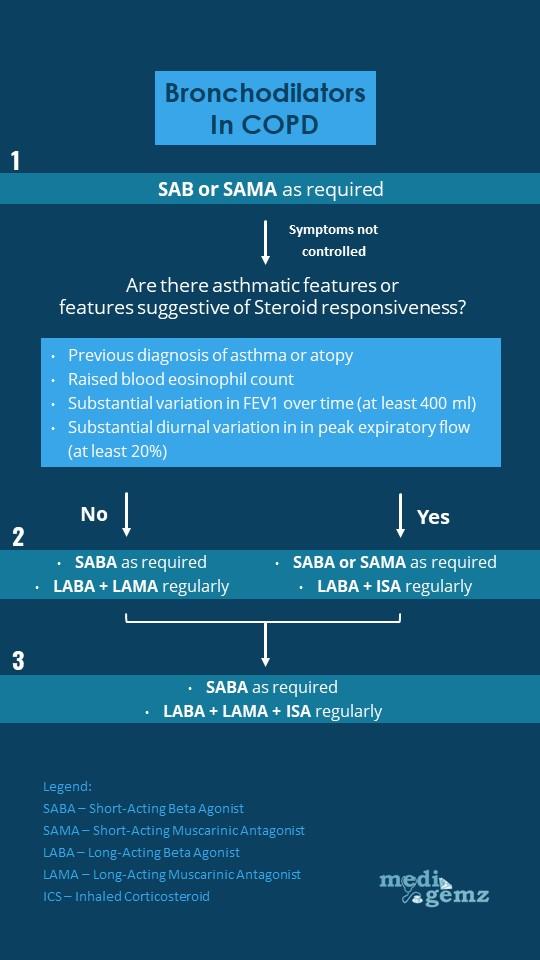
Bronchodilator Therapy
- First-line treatment with short-acting beta2-agonist (SABA) or short-acting muscarinic antagonist (SAMA).
- Second-Line treatment: For patients who remain breathless or have exacerbations despite using short-acting bronchodilators, the next step is determined by whether the patient has “Asthmatic features/features suggesting steroid responsiveness.” There are a number of criteria NICE suggests to determine whether a patient has asthmatic/steroid-responsive features:
- Any previous, secure diagnosis of asthma or of atopy
- A higher blood eosinophil count
- Substantial variation in FEV1 over time (at least 400 ml)
- Substantial diurnal variation in peak expiratory flow (at least 20%)
- There is 1 of the 2 choices based on the assessment of asthmatic features and features suggesting steroid responsiveness.
- If there are no asthmatic features/features suggesting steroid responsiveness:
- Add a long-acting beta2-agonist (LABA) + long-acting muscarinic antagonist (LAMA)
- If already taking a SAMA, discontinue and switch to a SABA
- If there are Asthmatic features/features suggesting steroid responsiveness:
- LABA + Inhaled corticosteroid (ICS)
- If patients remain breathless or have exacerbations offer triple therapy i.e. LAMA + LABA + ICS
- If the patient is already taking a SAMA, discontinue and switch to a SABA
- NICE recommend the use of combined inhalers where possible
Oral Theophylline
- NICE only recommends theophylline after trials of short and long-acting bronchodilators or for people who cannot use inhaled therapy.
- The dose of Theophylline should be reduced if macrolide or fluoroquinolone antibiotics are co-prescribed to reduce the risk of Theophylline toxicity. (Macrolides and fluoroquinolones are enzyme inhibitors and are commonly prescribed antibiotics for patients with COPD exacerbations.)
Oral Prophylactic Antibiotic Therapy
Consider azithromycin (usually 250 mg 3 times a week) for people with COPD if they:
- do not smoke and
- have optimized non-pharmacological management and inhaled therapies, relevant vaccinations and (if appropriate) have been referred for pulmonary rehabilitation and
- continue to have 1 or more of the following, particularly if they have significant daily sputum production:
- Frequent (typically 4 or more per year) exacerbations with sputum production
- Prolonged exacerbations with sputum production
- exacerbations resulting in hospitalization.
- Before offering prophylactic antibiotics, ensure that the person has had:
- sputum culture and sensitivity (including tuberculosis culture), to identify other possible causes of persistent or recurrent infection that may need specific treatment (for example, antibiotic-resistant organisms, atypical mycobacteria or Pseudomonas aeruginosa)
- training in airway clearance techniques to optimize sputum clearance
- a CT scan of the thorax to rule out bronchiectasis and other lung pathologies.
- Before starting azithromycin, ensure the person has had:
- an electrocardiogram (ECG) to rule out prolonged QT interval and
- baseline liver function tests.
Mucolytics
- Mucolytics should be considered in patients with a chronic productive cough and continued if symptoms improve.
Cor-pulmonale
- Features to suggest Cor-pulmonale include peripheral oedema, raised jugular venous pressure (JVP), systolic parasternal heave, and loud P2.
- Continue optimized COPD treatment.
- Help in smoking cessation.
- Use a loop diuretic for oedema.
- Consider long-term oxygen therapy for patients with indiction.
- Do not use ACE-inhibitors, calcium channel blockers and alpha-blockers and Digoxin (unless there is AF) to treat cor-pulmonale caused by COPD.
Factors which may improve survival in patients with stable COPD
- Smoking cessation is the single most important intervention for patients who are still smoking.
- Long-term oxygen therapy (LTOT) in patients who fit the criteria.
- Lung volume reduction surgery in selected patients.
great publish, very informative. I ponder why the other specialists of this sector don’t notice this. You must proceed your writing. I’m sure, you have a great readers’ base already!
I think this is a genuine great article.Really thank you! in reality Great.