Electrocardiography (ECG) is one of the most common bedside diagnostic tools, used by health care providers. You must be aware of the standard protocol of its interpretation, which is, calculating the rate, checking rhythm, axis, bundle branch block, and then checking individual waves, intervals and segments. But this post gives you some very useful points that you might have not known before. These tips will surely take your ECG interpretation skills to the next level.
Tip # 1 - Amplitude of Waves
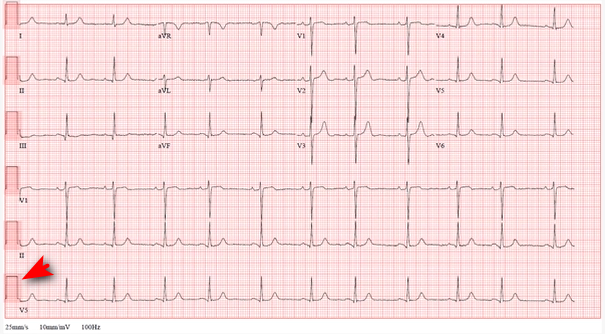
Many times you may come across ECGs, where ECG waves are either too small or too big. Before commenting on wave amplitudes, see the voltage calibration bar at the start of every ECG. This bar denotes the voltage at which the ECG is recorded.
The standard voltage at which ECG is recorded worldwide is 1 mV. This is equivalent to the height of 10 small (or 2 large squares) on ECG. Machine voltage lesser or more than this setting will record an ECG, where the waves will appear smaller or larger, respectively.
So next time you see a high or low amplitude QRS complex, before saying its hypertrophy of ventricles or the patient is having low voltage ECG, check the voltage at which the ECG had been recorded.
Tip # 2 - Speed of Machine
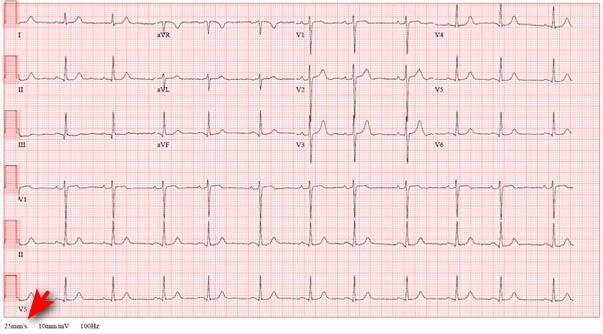
Standard machine speed at which every ECG is recorded is 25 mm/second. The speed is printed on the ECG strip (as shown in the figure).
If the machine speed is set more than this, the waves will be farther from one another & appears as bradycardia erroneously, and vice versa. This can make you interpret wrongly.
So if you come across an ECG showing bradycardia/tachycardia, while the patient looks otherwise stable normal measured pulse, check the ECG recording speed.
Tip # 3 - Correlate ECG Clinically
When you come across an abnormal ECG, correlate it clinically with the patient’s condition. Sometimes, apparent ST elevation can be disregarded as high take-off in young, fit individuals with no typical symptoms, while the same changes may need further workup and evaluation in an elderly patient with risk factors for IHD.
Clinical correlation is also important in a busy emergency department, where too many ECGs are done in a short span. So, check patients’ symptoms and correlate ECG, before rushing into telling a patient sitting comfortably in bed, that he has a myocardial infarction. While in fact, the ECG was that of another patient on the side bed.
Tip # 4 - Rhythm Strip in ECG
Make it a habit to check the rhythm strip, for calculation of rate and checking rhythm. All modern ECG machines, automatically record the rhythm strip, which is lead-II. In places where still older machines are used, ask the technician to manually record long lead II (rhythm strip).
This strip is useful in calculating rates in atrial fibrillation. The number of QRS complexes is counted in 6 seconds strip, and then this number is multiplied by 10 to get the heart rate per minute.
Tip # 5 - Serial ECGs
Never rely on a single normal ECG in patients with chest pain presenting shortly after the onset of symptoms. Detain the patient for some time in the emergency department and do serial ECGs to see the development of any new ECG changes. This is particularly important in patients having risk factors for coronary artery disease.
Please watch this video for revising these points!
My brother suggested I might like this web site. He was entirely right. This post actually made my day. You cann’t imagine simply how much time I had spent for this info! Thanks!