This is a sleep disorder in which there is disturbed sleep at night time and the patient has recurrent apneic or hypopnea episodes in between. This leads to interruptions in normal sleep and patient is somnolent, lethargic despite having apparently adequate sleep.

Pathophysiology
Obstructive sleep apnea-hypopnea syndrome (OSAHS) is a sleep disorder in which there is a physical narrowing of the upper airway, usually at the level of the soft palate.
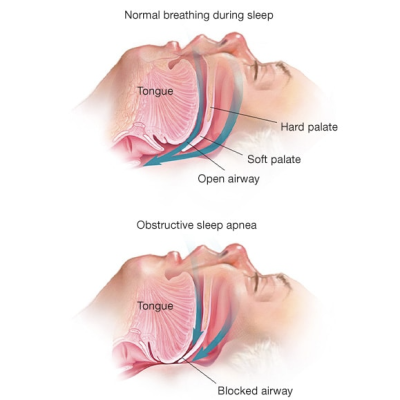
Normally, during inspiration, there is a build-up of negative air pressure in the pharynx and there is a tendency for the collapse of the upper airway. During wakefulness, upper airway dilating muscles (palatoglossus and genioglossus) contract and keep the airway patent. During sleep, however, the tone of these muscles decreases leading to a potential for upper airway collapse during inspiration. If there is additional anatomical upper airway narrowing, obstructive sleep apnea-hypopnea develops.
There are recurrent upper airway obstructions during sleep which are sufficient enough to cause sleep fragmentation and daytime sleepiness.
Clinical Features
– Excessive daytime sleepiness – the cardinal symptom
– Fatigue
– Weight gain
– Erectile dysfunction
– Morning headaches
– Apnea episodes and snoring – observed by the spouse
– Difficulty with concentration, impaired cognitive function and work performance
– Irritability/Depression
– Nocturia
– Plethoric face (erythrocytosis is common)
– Systemic hypertension – develops due to recurrent increased sympathetic stimulations during apnea/hypopnea episodes
– Pulmonary hypertension/corpulmonale
Diagnosis
History of daytime excessive sleepiness, and snoring at night is typical. Daytime tendency to fall asleep can be assessed quantitatively with a questionnaire, like given below:
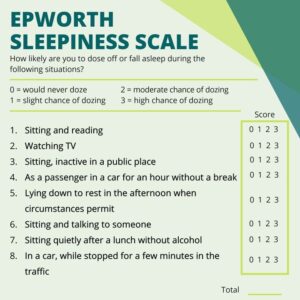
Provided that sleepiness does not result from inadequate sleep time, anyone who repeatedly falls asleep during the day should be referred for a sleep assessment.
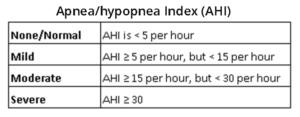
Polysomnography (Overnight studies of breathing, oxygenation, and sleep quality) is diagnostic. The severity of OSAHS is determined by the number of apnoea/hypopnoea per hour of sleep (apnoea/hypopnoea index, AHI).
Apnoea = a 10-second or longer breathing pause
Hypopnoea = a 10-second or longer 50% reduction in ventilation that results in a 4% drop in arterial oxygen saturation.
Differential Diagnoses
– Narcolepsy is a rare cause of sudden-onset sleepiness.
– Idiopathic hypersomnolence occurs in younger individuals and is characterized by long nocturnal sleep.
– COPD
– Alcohol or sedative abuse
– Hypothyroidism
– Seizure disorder
Management
Weight loss in overweight or obese patients. Weight loss decreases the AHI and blood pressure, and improves overall health and quality of life.
Avoidance of hypnotics – alcohol or sedating medication shall be avoided.
Nocturnal continuous positive airway pressure (CPAP) – is the gold standard therapy for the majority
of patients with OSAHS. There is dramatic improvement of symptoms. Main issue is the compliance due intolerance of tight fitting mask.
Mandibular advancement devices – are considered in those patients who cannot tolerate CPAP.
CNS stimulant drugs – such as Modafinil – is used sometimes as adjunctive therapy to conventional treatment in patients to help with their excessive daytime sleepiness.
Surgical procedures – in rare cases uvulopalatopharyngoplasty, nasal septoplasty etc.
Avoid driving – Since the major hazard to patients and those around them is traffic accidents. DVLA shall be informed and drivers must be strongly advised not to drive until treatment has relieved their sleepiness.
Share Your Thoughts in the comments below. We would love to know about your valuable experience if you have already been through this exam.