Introduction
Sarcoidosis is a multisystem, granulomatous disease of unknown etiology.
It is characterized by non-caseating granulomas.
Lung being most commonly affected (in over 90% cases), sarcoidosis can involve any organ of the body.
Clinical features
Accidental diagnosis – Sarcoidosis can be diagnosed as an accidental finding as bilateral hilar lymphadenopathy (BHL) on chest radiograph in an asymptomatic individual doing chest X-ray for some other reason.

Pulmonary disease – present in a more insidious manner with cough, exertional breathlessness and radiographic infiltrates.
Chest auscultation is often surprisingly unremarkable. If there is pulmonary fibrosis, which occurs in around 20% of cases of pulmonary sarcoidosis, you may be able to hear dry crackles over the affected areas.
Lofgren’s syndrome – Sarcoidosis can sometime present, usually in young women, with an acute illness characterized by erythema nodosum, peripheral arthropathy, uveitis, bilateral hilar lymphadenopathy, lethargy and occasionally fever. This is called Lofgren’s syndrome.
Complications – Rarely, sarcoidosis may present with complications such as bronchiectasis, aspergilloma, pneumothorax, pulmonary hypertension and cor-pulmonale.
Laboratory tests
Bronchoscopy may demonstrate a ‘cobblestone’ appearance of the mucosa.
Bronchial & transbronchial biopsies usually show non-caseating granulomas.
Bronchoalveolar lavage (BAL) fluid typically contains an increased CD4:CD8 T-cell ratio.
Complete blood counts (CBC) – Lymphopenia is characteristic.
Liver function tests (LFTs) – may be mildly deranged.
Hypercalcaemia may be present. If present, this is due to the increased formation of calcitriol by alveolar macrophages. It is particularly prevalent in patients who have been exposed to strong sunlight.
Hypercalciuria may also be present and can lead to nephrocalcinosis.
Angiotensin-converting enzyme (ACE) levels may provide a non-specific marker of disease activity and can assist in monitoring the clinical course.
Radiology
Chest radiography has been used to stage sarcoidosis into 5 stages.
Stage 0 – Normal chest radiograph
Stage I – Hilar or mediastinal nodal enlargement only
Stage II – Nodal enlargement + Parenchymal disease
Stage III – Parenchymal disease only
Stage IV – End-stage lung disease (Pulmonary Fibrosis)
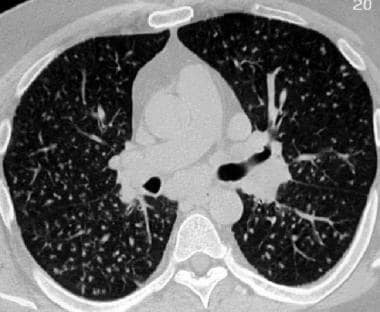
High-resolution CT scan (HRCT) chest
Characteristic HRCT appearances include reticulonodular opacities that follow a peri-lymphatic distribution, centred on bronchovascular bundles and the subpleural areas.
Pulmonary Function Tests (PFTs)
PFTs may show restrictive defect accompanied by impaired gas exchange in patients with pulmonary infiltrates.
Exercise tests may reveal oxygen desaturation.
Bronchoscopy

Positron Emission Tomography (PET) scan
PET scanning can detect extrapulmonary disease.
Diagnosis of Sarcoidosis
You may face one of the following scenarios. In the first 2 cases, there is no need for a histopathological diagnosis.
1. Erythema nodosum with BHL on chest X-ray is often sufficient for a confident diagnosis, without a need for tissue biopsy.
2. Typical presentation along with classical HRCT features is also sufficient for diagnosis.
3. In other presentations, the diagnosis should be confirmed by histological examination of the involved organ.
Management
Lofgren’s syndrome – Treat Lofgren’s syndrome with NSAIDs. A short course of glucocorticoids is needed occasionally. There is spontaneous remission in the majority.
Steroids in sarcoidosis –
Prednisolone is indicated in hypercalcaemia, pulmonary impairment, renal impairment and uveitis. Starting dose of 20–40 mg/day should be commenced immediately.
Topical glucocorticoids are used in mild uveitis.
Inhaled glucocorticoids can be used to shorten the duration of systemic glucocorticoids in asymptomatic parenchymal sarcoid.
Immunosuppressants –
Methotrexate, Azathioprine and specific Tumour Necrosis Factor-alpha (TNF-α) inhibitors are used in patients with severe disease.
Chloroquine, Hydroxychloroquine and low-dose Thalidomide are useful in cutaneous sarcoid with limited pulmonary involvement.
Avoidance of sun exposure – educate patients to avoid strong sunlight as it can hypercalcemia and affect renal functions.
Poor prognostic factors in sarcoidosis
Age over 40
Afro-Caribbean ethnicity
Persistent symptoms for more than 6 months
Involvement of >3 organs
Lupus pernio
Stage III/IV on chest X-ray
hydroxychloroquine chloroquine prophylaxis
Greetings from Ohio! I’m bored at work so I decided to browse your website on my iphone during lunch break. I really like the info you present here and can’t wait to take a look when I get home. I’m shocked at how quick your blog loaded on my cell phone .. I’m not even using WIFI, just 3G .. Anyhow, wonderful blog!
Does your blog have a contact page? I’m having trouble locating it but, I’d like to send you an email. I’ve got some suggestions for your blog you might be interested in hearing. Either way, great website and I look forward to seeing it grow over time.
Dude these articles were really helpful to me. Thanks a lot.