Hyponatremia is a very common abnormality encountered in daily clinical practice, especially in critically ill inpatients. This post will give you an approach to interpreting hyponatremia in a methodical way.
Hyponatremia is said to be present when serum Na+ is < 135 mmol/L.
From Physiology basics, we know that Sodium is the major extracellular cation. Changes in serum sodium are always accompanied by alterations in water status, mainly extracellular volume.
In hyponatremia, fundamentally, there is greater retention of water relative to sodium, and therefore serum osmolality will be low.
Pathophysiology
A variety of causes can lead to hyponatremia. To make it easy, causes of hyponatremia are best categorized according to the extracellular fluid volume status. Determining the volume status of a patient is necessary because this helps us narrow down the differential diagnosis of hyponatremia.
As we know that there are 3 possible volume statuses. Hypovolemia, Euvolemia or Hypervolemia.
So, the patient with hyponatremia will have at least one of these three statuses. Whatever the patient’s volume status, hyponatremia has occurred because there is more water relative to the sodium.
Before proceeding further, let me highlight another important aspect… Calculate Osmolality. Why??? Let me explain!!!
Whenever you come across a lab report of hyponatremia, it is pertinent to note that sometimes you may get ‘false’ hyponatremia in test results. This may occur either due to an increased serum osmolality or may be due to lab artefacts.
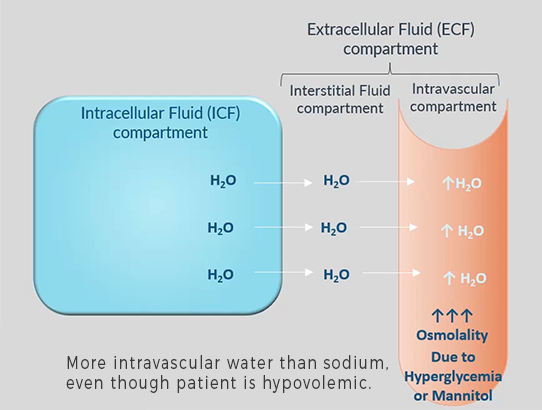
1. Hyperosmolality causes an osmotic shift of water from intracellular & interstitial space to intravascular space (as shown in the figure), leading to a relatively increased water amount to sodium. This situation may be seen in severe hyperglycemia or with the use of osmotically active substances such as Mannitol. In these situations, serum osmolalilty will be high (Hypertonic).
2. Artefactual causes of hyponatraemia, on the other hand, include severe hyperlipidaemia or hyperproteinaemia (Hypergammaglobulinemia). Here the aqueous fraction of the serum specimen is reduced because of the volume occupied by the macromolecules. This artefact is seen only with the use of certain assay technologies. Since there is no actual change in body water or sodium status, this hyponatremia is called ‘Pseudohyponatremia’. In this case, serum osmolality will be normal (Isotonic).
Having explained the importance of osmolality affecting the lab result, if we get hyponatremia in a patient, we shall verify whether the low sodium we are dealing with is actually low sodium (in true hyponatremia, serum osmolality is low – Hypotonic) or is it the result of the above-mentioned phenomenon (Hypertonic or Isotonic Hyponatremia). Calculate the serum osmolality by this equation:
Serum Osmolality = 2 [Na+] + Glucose (mmol/L) + Urea (mmol/L)
To convert values from mg/dl to mmol/L, divide by 18 for glucose, and by 2.8 for urea.
Normal serum osmolality ranges between 275 – 295 mOsm/Kg. If osmolality calculated is < 275 mOsm/Kg, hyponatremia is true and not the result of lab artefacts or hyperosmolality.
Once established that it is true hyponatremia, assess the volume status of the patient and see whether the patient is hypovolemic, normovolemic or hypervolemic.
Hypovolemic Hyponatremia: If the patient is hypovolemic, there is depletion of sodium and water but the sodium deficit exceeds the water deficit, causing hypovolaemia and hyponatraemia. It is seen in GI losses such as vomiting or diarrhoea, use of diuretics especially thiazides, third spacing of fluids, burns, adrenocortical insufficiency, cerebral salt wasting and sodium losing nephropathy. You will find symptoms and signs of hypovolemia and the cause of sodium loss is apparent from history.
Symptoms: Thirst, Dizziness on standing, Weakness
Signs: Postural hypotension, tachycardia, prolonged capillary refill time (CRT), dry mouth, reduced skin turgor, reduced urine output, weight loss delirium, stupor
Hypervolemic Hyponatremia: In hypervolemia or fluid overload, excess water retention has occurred due to sodium retention, and there is volume expansion. This is seen in heart failure, liver cirrhosis or nephrotic syndrome. So here the cause of hyponatremia is usually obvious from the clinical evaluation of the patient.
Euvolemic Hyponatremia: Lastly, in hyponatremic patients with normal volume (euvolemia), there is no major disturbance of body sodium content and water content is relatively more compared to sodium due to some reason.
Excess body water may be the result of abnormally high intake, either orally (primary polydipsia) or as a result of medically infused fluids – intravenous dextrose solutions or by absorption of sodium-free bladder irrigation fluid after prostatectomy.
Water retention also occurs in the syndrome of inappropriate secretion of antidiuretic hormone, or vasopressin (SIADH). In this condition, an endogenous source of vasopressin (either cerebral or tumour-derived) promotes water retention by the kidney in the absence of an appropriate physiological stimulus. The clinical diagnosis requires the patient to be euvolemic, with no evidence of cardiac, renal or hepatic disease potentially associated with hyponatraemia. Other non-osmotic stimuli that cause the release of vasopressin (pain, stress, nausea) should also be excluded. Supportive laboratory findings are shown in fig below.
Other causes of euvolemic hyponatremia include hypothyroidism, pure glucocorticoid deficiency, tea and toast diet or beer potomania.
To summarize, please take a look at following table:
| Low Na+ & Low Serum Osmolality < 275 mOsm/Kg | |||
| Hypovolemic Hyponatremia | Euvolemic Hyponatremia | Hypervolemic Hyponatremia | |
| Total body water | ↓ | ↑ | ↑↑ |
| Total body sodium | ↓↓ | ↔ | ↑ |
| Causes | GI losses –Vomiting, Diarrhea, Diuretics – Thiazides Adrenocortical insufficiency Cerebral salt wasting Sodium losing Nephropathy | Primary polydipsia SIADH Hypothyroidism Glucocorticoid deficiency Beer potomania | Congestive Heart Failure Hepatic Cirrhosis Nephrotic Syndrome Renal failure |
Clinical features
Hyponatremia is often asymptomatic but may be associated with profound disturbances of cerebral function. The symptoms of hyponatremia depend on the speed at which it develops and its severity. The symptoms are more related to the speed at which it develops than its severity.
Normally intracellular and extracellular osmolality stays equal, allowing free movement of water in both directions, with no net increase in a single direction. But, when hyponatremia develops acutely, plasma osmolality falls.
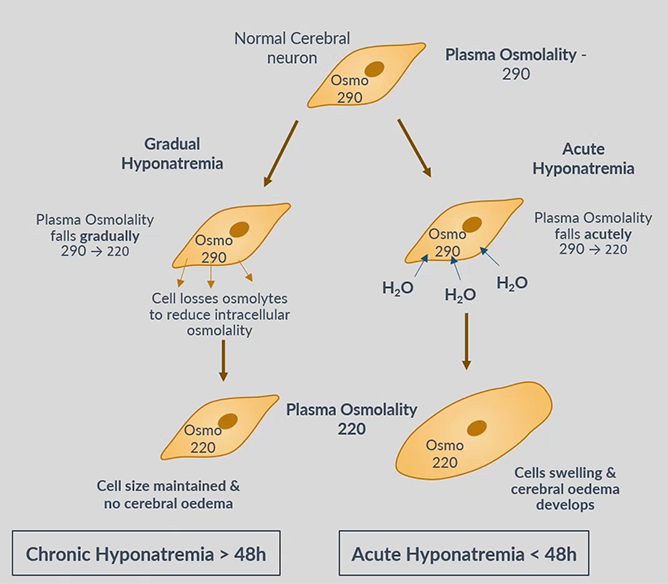
Cells have no time to adjust to this difference in intercompartmental osmolality and water rapidly flows into cerebral cells, causing them to become swollen and ischemic.
On the other hand, when hyponatremia develops gradually, cerebral neurons have time to respond by reducing intracellular osmolality, through excreting potassium and reducing the synthesis of intracellular organic osmolytes. The osmotic gradient between two compartments is reduced and therefore there is no intracellular shift of water. This process takes about 24–48 hours.
Therefore, hyponatremia is classified as Acute, if it develops in < 48 hours, and Chronic, if it develops in > 48 hours.
Hyponatraemia can also be defined as Mild, Moderate & Severe based on biochemical findings or on the degree of severity of symptoms.
Serum Na+
- Mild hyponatremia 130 – 135 mmol/L
- Moderate hyponatremia 125–129 mmol/L
- Severe hyponatremia < 125 mmol/L
Mild hyponatremia may not have any symptoms, moderate may present with nausea, headache and delirium, while severe hyponatremia with vomiting, somnolence, seizures, coma and cardiorespiratory arrest.
Diagnostic Approach
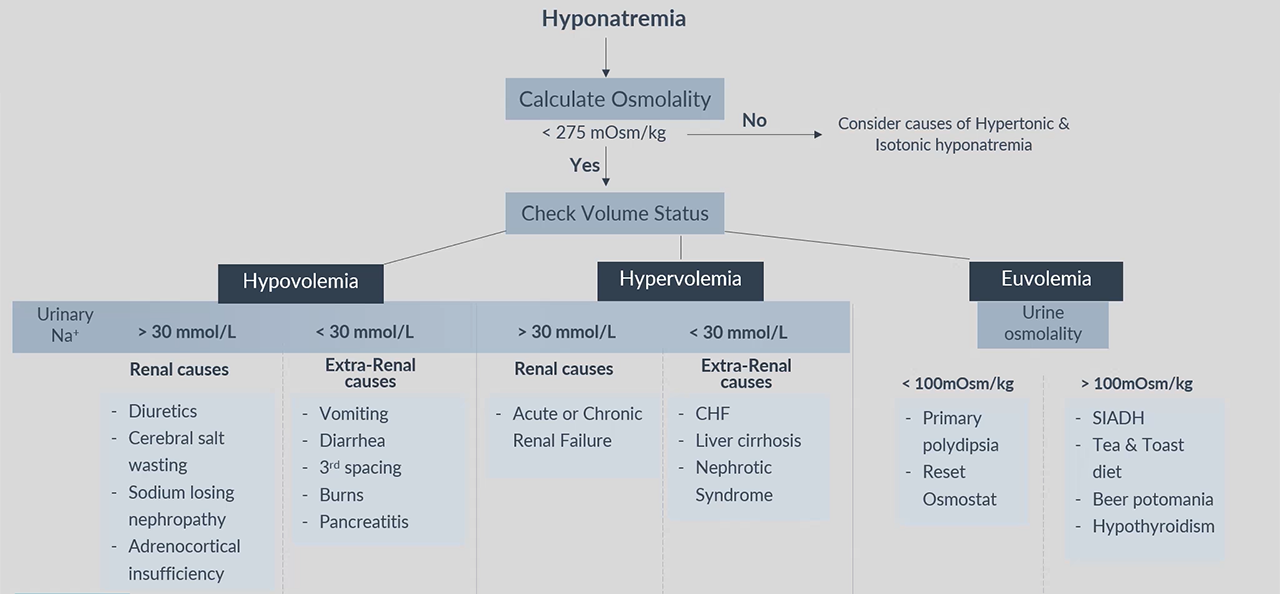
After checking and confirming True hyponatremia by checking plasma Osmolality, grouping the patient according to volume status can let you easily arrive at the cause from clinical history & examination. Serum and urine electrolytes and osmolality are usually the only tests required to clarify the underlying cause.
In hypovolemic and hypervolemic groups, low urinary sodium concentration (< 30 mmol/L) indicate extrarenal causes of sodium loss and high urinary sodium concentration (> 30 mmol/L) occurs in patients with excessive renal sodium loss.
In the euvolemic group, urine osmolality <100 mOsm/kg points toward high water intake and reset osmostat. On the other hand, >100mOsm/Kg urine osmolality indicate other causes in this group of patients.
Following is an algorithm for the clinical assessment of patients with hyponatremia:
Management
- Correction of Hyponatremia
The treatment of hyponatraemia is critically dependent on its rate of development, severity, presence of symptoms and underlying cause.
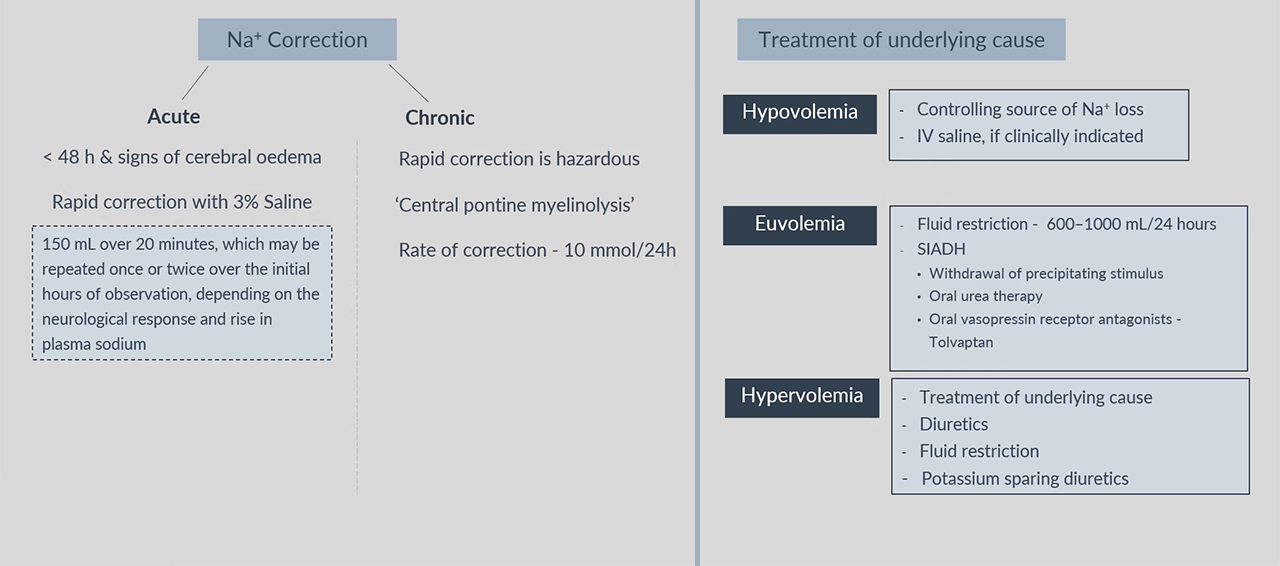
If hyponatraemia has developed rapidly (< 48 hours) and there are signs of cerebral oedema, such as obtundation or convulsions, sodium levels should be restored rapidly to normal by infusion of hypertonic (3%) sodium chloride. A common approach is to give an initial bolus of 150 mL over 20 minutes, which may be repeated once or twice over the initial hours of observation, depending on the neurological response and rise in plasma sodium.
Rapid correction of hyponatraemia that has developed more slowly (> 48 hours) can be hazardous, since brain cells adapt to slowly developing hypo-osmolality by reducing the intracellular osmolality, thus maintaining normal cell volume. Under these conditions, an abrupt increase in extracellular osmolality can lead to water shifting out of neurons, abruptly reducing their volume and causing them to detach from their myelin sheaths. The resulting ‘myelinolysis’ can produce permanent structural and functional damage to mid-brain structures and is generally fatal. The rate of correction of the plasma Na concentration in chronic asymptomatic hyponatraemia should not exceed 10 mmol/L/24 hrs, and an even slower rate is generally safer.
2. Treatment of the underlying cause
The underlying cause should also be treated.
For hypovolaemic patients, this involves controlling the source of sodium loss, and administering intravenous saline if clinically warranted.
Patients with euvolemic hyponatraemia generally respond to fluid restriction in the range of 600–1000 mL/24 hrs, accompanied where possible by withdrawal of the precipitating stimulus (such as drugs causing SIADH). In patients with persistent hyponatraemia due to prolonged SIADH, oral urea therapy (30–45 g/day) can be used, which provides a solute load to promote water excretion. Oral vasopressin receptor antagonists such as tolvaptan may also be used to block the vasopressin-mediated component of water retention in a range of hyponatremic conditions, but concerns exist with regard to the risk of overly rapid correction of hyponatraemia with these agents.
Hypervolaemic patients with hyponatraemia need treatment of the underlying condition, accompanied by the cautious use of diuretics in conjunction with strict fluid restriction. Potassium-sparing diuretics may be particularly useful in this context when there is significant secondary hyperaldosteronism.
Best view i have ever seen !
Best view i have ever seen !
Best view i have ever seen !